11 Aug Malagasy-Led Study Advances Innovative Methods For Understanding Geographic Access To Health Care
Members of the PIVOT team trek to the village of Ambalapaiso, which is located 13 kilometers from the nearest health facility.
With more than three and a half billion people lacking access to essential health services, most countries around the globe, including Madagascar, have renewed their commitment to Universal Health Coverage (UHC).
One of the most challenging barriers to achieving UHC in Madagascar is geography, where 60% of the population lives more than 5 kilometers from the nearest health facility. Surprisingly, however, the geography of health access remains poorly understood. Health systems, facility locations, and community health programs are designed with limited understanding of the real geographic barriers to care. Climate, waterways, land use, terrain, and physical distance are all central to determining whether a sick child receives care or a pregnant woman delivers at a facility.
So how can we update modern analytics to break down geographic barriers to care?
A new study led by PIVOT researcher Dr. Felana Ihantamala, also a postdoctoral fellow at Harvard Medical School, has achieved a very precise understanding of local geographic accessibility to health care in Ifanadiana District, Madagascar. The study includes establishing estimates of distance to care for every single household in the area in order to support the programs that deliver health care to remote populations. Beyond improving the precision of previous methods for assessing geographical accessibility, the study has made all the results available for operational use in the field by PIVOT staff and other local health actors in the region via interactive e-health tools.
Recently published in the International Journal of Health Geographics, the study provides a comprehensive picture of the geographic challenges faced by the population to reach the health services they need, be it from the nearest health center or community health worker.
(You can access the full study HERE.)
Dr. Ihantamalala, a health geographer by training, recognizes that, “to optimize local interventions, a very precise understanding of the local geography is necessary to identify populations with poor geographic accessibility to health facilities, to plan field missions, or set up itineraries for community health workers that are doing proactive care, and outreach teams involved in [mobile] vaccination campaigns.”
(Learn more about Felana in her spotlight profile, HERE.)
However, implementation efforts are currently limited by a lack of basic geographic information (e.g. footpaths, residential areas, households) in most rural areas of Madagascar. To solve this in Ifanadiana District, PIVOT partnered with the Humanitarian OpenStreetMap Team and Institut de Recherche pour le Developpement to complete a participatory mapping exercise that ultimately identified more than 100,000 buildings, 5,000 residential areas, 13,000 hectares of rice paddies, and a network of nearly 15,000 miles of footpaths.
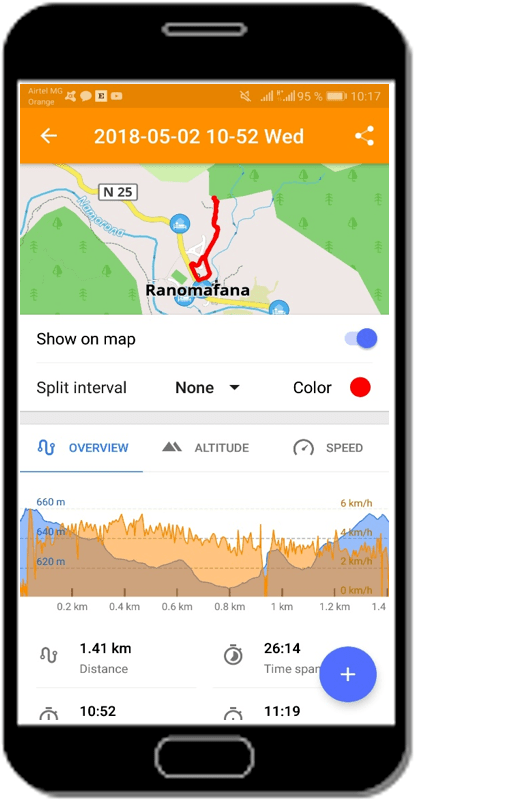
Through remote sensing work and GPS measurements, our team is now able to generate accurate estimates of travel time between virtually any two points in the district. To facilitate the operational use of the results of this research by healthcare providers and programmatic teams, the research team developed a web application that is available on PIVOT’s new research dashboard. Beyond this, field workers can also generate accurate directions to any point in Ifanadiana District without internet access (which is scarce throughout the region) using the free “OSMAnd” app on smartphones and tablets.
(Check out the dashboard for yourself, HERE.)
Besides its scientific relevance, this study has contributed to local research capacity-building. PIVOT Associate Scientific Director and senior author of the article, Dr. Andrés Garchitorena, adds that “this work was possible thanks to the contribution of three Malagasy master’s students in GIS and remote sensing who did their thesis on this project, and to several ‘mapathons’ organized at the University of Fianarantsoa and with members of the OpenStreetMap community.”
We know that this type of locally-led scientific approach to solve context-specific barriers to health care can be key tools for achieving UHC in rural areas of the developing world, and look forward to the direct impact that this study will have on PIVOT’s program design and outcomes.